How Much Do Doctors Actually Make?
Stop relying on the average doctor salary. We break down the pay difference between specialties and how RVUs & procedures impact your compensation.

So you want to be a dermatologist. You love the idea of popping pimples by day and curing skin cancer by night. Okay, maybe not quite. Let’s debunk the public perception myths of dermatology and give it to you straight. This is the reality of being a dermatologist.
Welcome to our So You Want to Be series, where we highlight a specific specialty within medicine to help you decide if it’s a good fit for you. For this episode, we’re bringing our Insider expert to you. Dermatologist Dr. Austin Johnson will join us to give you a glimpse into the world of dermatology.
Let’s get started.
Dermatology is the specialty that manages diseases of the skin, hair, and nails, combining both medical and procedural aspects. Many think skin is relatively straightforward, but it’s far more complicated than it seems. A dermatologist can identify and treat more than 3,000 conditions, including eczema, psoriasis, and skin cancer, among others.
How might you describe dermatology to a 5-year-old?
Dr. Johnson: Think of your skin like a superhero suit covering the whole body. It keeps the germs out, helps you feel things like hugs, and keeps you warm or cool. Sometimes, your skin gets grumpy. You might get an itchy spot, a rash, a bug bite, or even pimples. That’s where a dermatologist comes in. Dermatologists examine your skin closely, much like detectives. They might use a special magnifying glass or a tiny flashlight to get a better look. They may even take a little sample to look under the microscope. Your skin can often reveal how your body is functioning on the inside, and dermatologists can use that as a form of X-ray vision to help diagnose more than just skin conditions.
Dermatology falls within four main categories:
First up is medical dermatology, which deals with general dermatologic concerns, such as skin cancer, viral warts, acne, rosacea, hair loss, and various rashes. It also includes minor in-office procedures like injections, skin biopsies, and excisions.
General dermatology offers a predictable schedule and cases, combining fast-paced office visits with longitudinal patient continuity.
At academic institutions, you can also expect to manage more complex skin diseases, and there are often entire clinics dedicated to certain conditions or categories of disease, such as melanoma, cutaneous oncology, and vascular anomalies, to name a few.
But general dermatology is about much more than just acne. The conditions medical dermatologists treat are wide-ranging, including psoriasis, eczema, and various inflammatory, ulcerative, and blistering diseases that may require systemic medications or lifelong management.
Aesthetic dermatology primarily focuses on cosmetic concerns, including rhytides and wrinkles, volume loss, hyperpigmentation, textural changes, scar revisions, and redness, all through advanced cosmetic procedures and laser technologies. This is also clinic-based with in-office procedures.
Procedures include laser and chemical resurfacing, microdermabrasion, collagen fillers, Botox, sclerotherapy, body contouring, and scar revision.
Surgical dermatology centers on Mohs micrographic surgery, a precise technique used to treat skin cancer that involves examining the tissue under the microscope at intervals to determine if the cancer is entirely removed. Mohs surgeons don’t just do Mohs surgery, though. They often also perform simple excisions, as you would in general dermatology, as well as cosmetic dermatology procedures.
While this is as surgical as dermatology gets, it’s essential to understand that these are still clinic-based, in-office procedures. This doesn’t happen in the operating room. Patients generally only need local anesthetics, and the surgeons often interact with the patient throughout the surgery.
You’re also more likely to have repeat customers. Not only do these patients need follow-up monitoring for their excised skin cancers, but once you get skin cancer, you’re also at a higher risk of it recurring somewhere else, which means Mohs surgeons work closely with medical dermatologists to screen patients and biopsy anything worrisome.
Inpatient dermatologists work as consultants to primary services in the hospital, such as internal medicine, pediatrics, or surgery, which often manage hospitalized patients with primary or comorbid dermatologic conditions. These dermatologists function in various capacities, maintaining their own clinical practices while also being on call for the hospital.
There is a short list of dermatologic emergencies, and while there aren’t many, these are the dermatologists who would provide recommendations to the managing service.
Patients in this category can be very sick and develop skin diseases concurrently, or the skin disease can be a manifestation of a systemic disease, revealing the story of other underlying disease processes. Thus, inpatient dermatologists are well-versed in internal medicine as well as unique or complex skin conditions.
Dermatology is not all acne, eczema, and skin cancer, and it’s certainly not Dr. Pimple Popper. While it can be extremely gratifying to extract milia and laser away dyspigmentation, dermatologists don’t go into the field to get away from medicine.
That dermatologist you see for dark spots? They just got out of another room with a distraught family after sharing that their loved one has metastatic melanoma. The cosmetic dermatologist who just resurfaced your skin? Last week, they had to excise an invasive skin cancer that chewed all the way through the nose.
Dermatologists love what they do, but not every patient story ends in a triumphant cure.
While a solid work-life balance is one of the reasons why dermatology is one of the most competitive specialties out there, it’s not easy. At most, dermatologists are taught 2 weeks of dermatology in their 4+ years of medical school, and they’re lucky to get more than that in a typical intern year.
That means your so-called 9-to-5, which is really more like an 8-to-5, is followed by a 5-to-9 of reading, researching, and practicing procedures, which extends beyond residency.
Dr. Johnson: It seems that a new biologic medication is being introduced every year, which requires constant review of immunology, clinical trials, and attendance at academic conferences to stay up-to-date.
You know all those drug commercials that comprise roughly 80% of ad revenue on cable/satellite TV? Rheumatologists and dermatologists are often the ones sifting through the results to determine whether X or Y is right for you.
All that to say, dermatology is wonderful, but it is far from easy.
You don’t always get the answer in dermatology, even after dermoscopy, multiple skin biopsies, and an extensive laboratory workup. The art of dermatology is being comfortable with broad differential diagnoses characterized by subtle clinical and histologic differences and, more importantly, developing a therapeutic relationship with patients that can sustain multiple iterations of therapies over weeks, months, or even years.
While there are times when they can walk into a room and immediately diagnose a condition from six feet away, it’s when you dive headfirst into a holistic evaluation of the patient and critically appraise the literature to clinch a diagnosis that often drives a dermatologist.
As with all specialties, you must enjoy the bread and butter of your field. For dermatology, that means skin checks, also known as full-body skin exams. If you enjoy pattern analysis and finding clues, you are going to love nevi and rashes.
What’s something that surprised you about dermatology?
Dr. Johnson: Looking back, I was initially nervous about the rapid-fire visits, as one of my passions is spending enough time to make a genuine connection with someone who is often going through the scariest, most painful time in their life.
Fortunately, the fact that both the patient and I can often see what’s bothering them, as well as my ability to potentially diagnose and address it immediately, leads to a strong therapeutic bond that I felt was missing in other specialty contexts. Telling someone they don’t have cancer, taking such a cancer off, or even just making someone confident in the organ that defines their social and biological interactions with the rest of the world is often akin to lifting a visible and invisible weight off of those who need a win in life.
I believe that everyone has a gift to offer humanity, and I am proud to say that it is my job to give people the opportunity to share that gift, unshackled by judgment or pain. What’s better than a field where you can make such potential a reality for dozens of people a day?
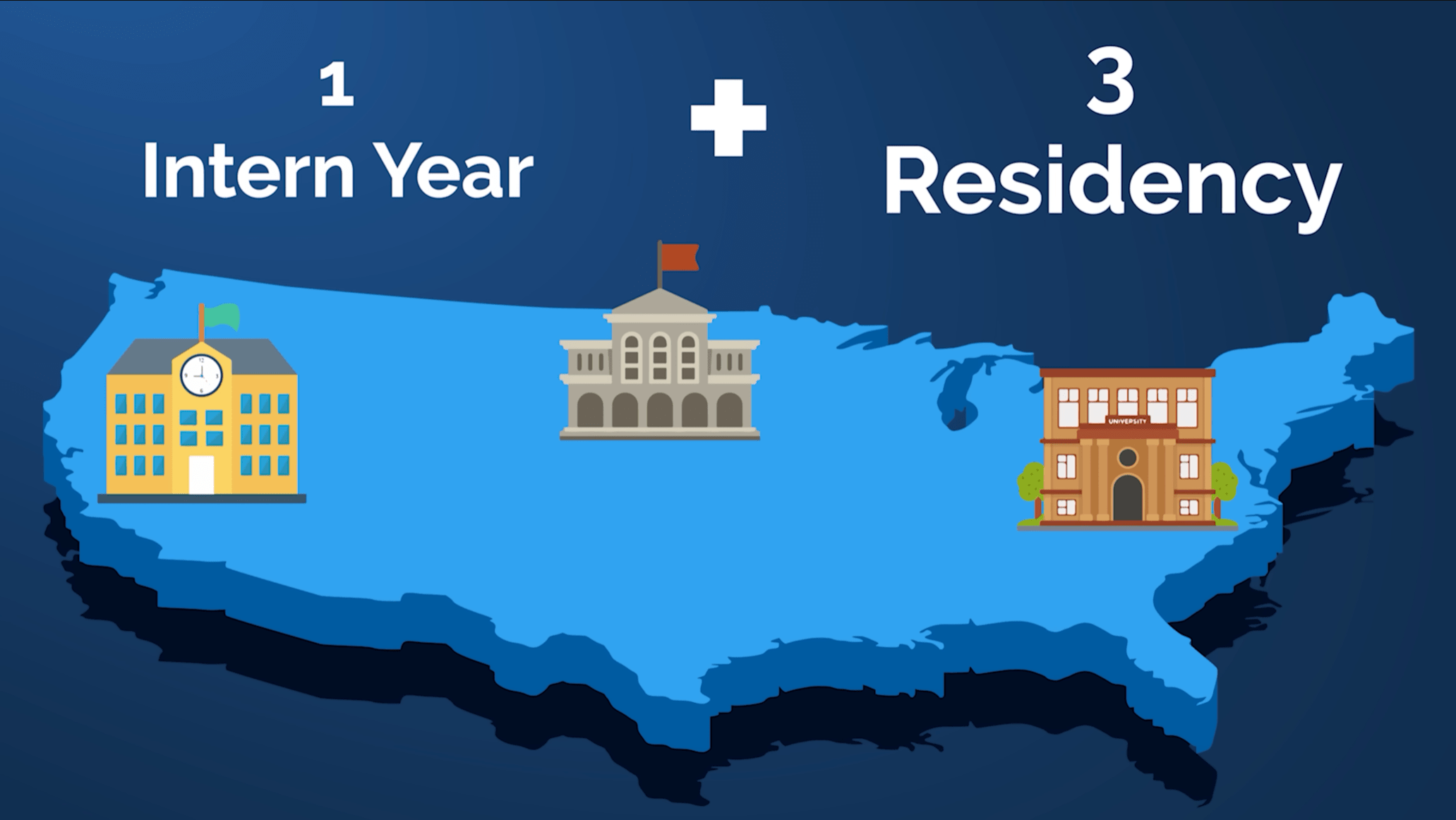
After finishing medical school, you’ll complete a one-year preliminary or transitional year. Collectively, this first year is referred to as your intern year. Oftentimes, prelims and TYs, as they are otherwise known, have little to no dedicated dermatology rotations, and instead are primarily cemented in the guise of what an intern in internal medicine would experience.
After that, the dermatology residency is 3 years. While there are technically combined 5-year internal medicine and dermatology programs, as of 2025, there are only a few in the entire country. The 1 + 3 model is much more typical, and while a few programs have linked prelims and dermatology program spots (with institutions such as Mayo boasting categorical programs, in which all 4 years fall under the same dermatology program), expect to potentially move across the country after finishing your intern year.
In terms of competitiveness, dermatology is consistently the first or second most competitive specialty in medicine, switching off with plastic surgery depending on the year. The average Step 2 CK score is 257, which is also the highest average Step 2 score of all categorical specialties.
Not only that, the average research items for newly christened derm residents is 27.7, the third-highest of any specialty, falling just behind plastic surgery at 34.7 and neurosurgery at 37.4~~, respectively.~~
If that sounds like a lot of research, that’s because it is. Research item averages have been increasing steadily for years. In 2020, the average research items for successful derm candidates was 19; in 2022, it was 20.9. Considering the 7.8 jump from 20.9 to 27.7 in research items between 2022 and 2024, it’s not hard to imagine that number easily cracking 30 by 2026.
For competitive specialties, you have to think ahead. That means making decisions early and determining what you need to do to become a competitive residency applicant.
But you don’t have to guess or wonder if you’re on track. The free tool at ResidencyPredictor.com shows you exactly where you stand compared to medical students who matched into your desired specialty. The prediction algorithm leverages the latest official match data to accurately predict your percentage odds of matching into that specialty.
It will even identify your relative weaknesses compared to the average person in that specialty, providing personal insights that will help you prepare before it’s too late.
See how your stats stack up for the specialties you’re most interested in. Unlock your competitiveness at ResidencyPredictor.com.
There are a handful of fellowships to choose from after residency, each lasting between one and two years.
Mohs micrographic surgery and dermatology oncology requires a 1- to 2-year fellowship. The prevailing joke among med students and residents is that these people wanted to become surgeons but didn’t want to sacrifice their work-life balance completely.
Compared to other dermatologists, the stereotype is that these physicians may have a lower tolerance for mistakes, work at a fast pace, and tend to be perfectionists with a similar attention to detail as plastic surgeons.
This is the specialty for dermatologists who enjoy constantly working with their hands and spending years fine-tuning a nuanced technique. For those who prefer excisions and biopsies over skin exams and topical steroids, Mohs surgery can be extremely appealing.
Cosmetic dermatology is a 1-year fellowship. However, unlike the other 3, as of 2025, there are no ACGME-accredited fellowships. Instead, the American Society for Dermatologic Surgery provides specific accreditation for cosmetic surgery programs scattered across the country. Compared to other sub-specialties, you’re more likely to end up in private practice, and being successful here requires an entrepreneurial spirit and expertise.
If you love working with kids as much as you love the largest human organ, then pediatric dermatology may be a good fit for you.
Pediatric dermatology is a one- or two-year fellowship for those who want to work exclusively with the pediatric population.
While generally clinic-based, this may require visits to the operating room, usually at academic institutions, as kids sometimes require sedation to tolerate procedures. Such a fellowship extends beyond typical eczema and acne, delving into unique conditions like blistering genodermatoses and vascular malformations.
Dermatopathology is a one- or two-year fellowship that follows the completion of either a pathology or dermatology residency. You may choose to focus exclusively on dermatopathology, or you may opt for a few days of clinic.
This is ideal for those who are highly visual, love recognizing patterns, and are passionate about histology. Plus, it offers a highly predictable schedule, as you’re looking through a microscope for most of the day.
Dr. Johnson: When people think about variety, they often gravitate toward fields with myriad subspecialties. One such archetype is internal medicine, in which you can specialize in the heart, lungs, colon, cancer, and everything else in between. However, I invite you to try to identify another specialty in which you need to master a microscope, a scalpel, and a disgruntled baby.
While many students and residents are worried about being pigeon-holed into one or the other, dermatology remains unique in that you can choose how specific to practice along the age and histologic spectrum of an organ that has many normal variations, as well as unique abnormalities.
Needless to say, you need to love the skin to practice dermatology. Still, despite the limited number of subspecialties on paper, no two medical, cosmetic, surgical, or pathology-leaning dermatologists are the same.
Don’t let this variety fool you, though. Dermatology is still a small field. Take pediatric dermatology, for example. Recent numbers suggest an average of 12 pediatric dermatologists enter the workforce annually, bringing the grand total to 300-400 across the entire United States as of 2023. The remaining sub-specialties often boast numbers above 1,000.
Taken together, in 2025, there were around 12,000 of us spread across the states. Taking that into perspective, consider all the major team sports players across the country, double it, and that’s how many dermatologists there are.
There’s a lot to love about dermatology. After all, it’s not the most competitive specialty around for nothing.
One of the strongest draws is the excellent lifestyle and work-life balance that isn’t afforded by most other disciplines within medicine. Given the outpatient nature, low acuity of medical conditions, limited call, and flexible workdays, dermatologists generally have more control over how and when they work than doctors in other specialties.
It also doesn’t hurt that dermatologists are highly compensated, earning an average of over $490,000 a year.
Dermatology is a highly visual field with equally high clinic volume that’s relatively fast-paced compared to other specialties. It’s also a field that allows for both medical and interventional encounters, which is ideal if you want to maintain continuity with patients while also regularly performing detail-oriented procedures.
You may not fully appreciate this now, especially if you’re early in your training, but dermatologists also spend less time on paperwork and administration than the average physician. That’s a huge deal.
And if you appreciate beauty in your work, in a visual way, cosmetic dermatology is an attractive option—no pun intended.
(What do you love most about dermatology and why did you choose it?).
Dr. Johnson: When I was in medical school, I could envision myself doing just about anything, which may sound surprising to those listening. However, when you look back at everything we covered today, I bet you can see why I dedicated my life to this specialty.
Beyond the ability to diagnose and excise that which is mysterious, bothersome, and even dangerous, it is the people behind the lesions and my colleagues and mentors that make this field the best. From shepherding someone with severe atopic dermatitis or psoriasis to a point where they achieve complete clearance from a biologic in a way some would otherwise deem magic to unmasking self-confidence in a teenager who was previously shackled by cystic acne through a personalized therapeutic ladder, I could not imagine choosing another field.
Of course, my parents, my brother, and most recently my wife are the the reason I am even speaking to you right now, so it shouldn’t be surprising at this point that dermatology was a perfect fit; as much as I want to be an excellent skin detective learned in the art of cutaneous intervention, so to do I want to be the best husband, sibling, son, and, eventually, father. What more could I ask for than a field that promotes the best of all worlds?
Dr. Johnson is one of many Dermatology Insiders at Med School Insiders. He’s helped hundreds of students navigate the ins and outs of applying to medical school. And after scoring in the 99.9th percentile on the MCAT, earning a 270+ Step 2 CK score, graduating from Stanford University School of Medicine, and matching into his top-choice residency program at Stanford Dermatology, you can rest assured that Dr. Johnson knows his stuff. He’s one of our most sought-after Insiders.
If you’re interested in working directly with Austin 1-on-1, sign up for his waitlist now.
But, of course, dermatology isn’t for everyone.
One of the most obvious downsides is how insanely competitive it is. Not only is it an extremely desirable specialty, but it’s also a small field with a limited number of residency spots. For this reason, many applicants find it necessary to take one or several years off during medical school to bolster their application with dermatology research, thereby improving their chances.
You may also find the field often misunderstood. Those who don’t fully understand and appreciate the specialty may dismiss your profession as being only skin-deep—think “Pimple Popper, M.D.” from Seinfeld.
Plus, typical surgeons usually won’t consider your work real surgery, even if you specialize in Mohs.
The fast-paced nature of the clinic is also a double-edged sword. On one hand, it’s exciting and engaging, but on the other hand, it may not suit all personalities, particularly if you want to spend more time with a patient.
How can you decide if dermatology is a good fit for you?
If you love pathologies related to the skin, enjoy working in a fast-paced clinic setting, like procedures but not to the extent of being in OR scrubs, and are willing to be a self-directed learner to tackle the immense amount of independent study required to be successful, then dermatology may be for you.
And finally, dermatology is one of the most competitive specialties, so you’ll need to be willing to put in the time and effort to become a top student. That translates to more than just high board scores, but also playing the research game, being a leader, and acing your clinical rotations.

Don’t forget to check out the free Residency Chance Predictor to find out how your stats stack up for your top-choice specialties at residencypredictor.com.
Stop relying on the average doctor salary. We break down the pay difference between specialties and how RVUs & procedures impact your compensation.

Are you built for the Emergency Department? We reveal the 6 signs that prove you’re destined to succeed in emergency medicine.
This Post Has One Comment
thanks for info